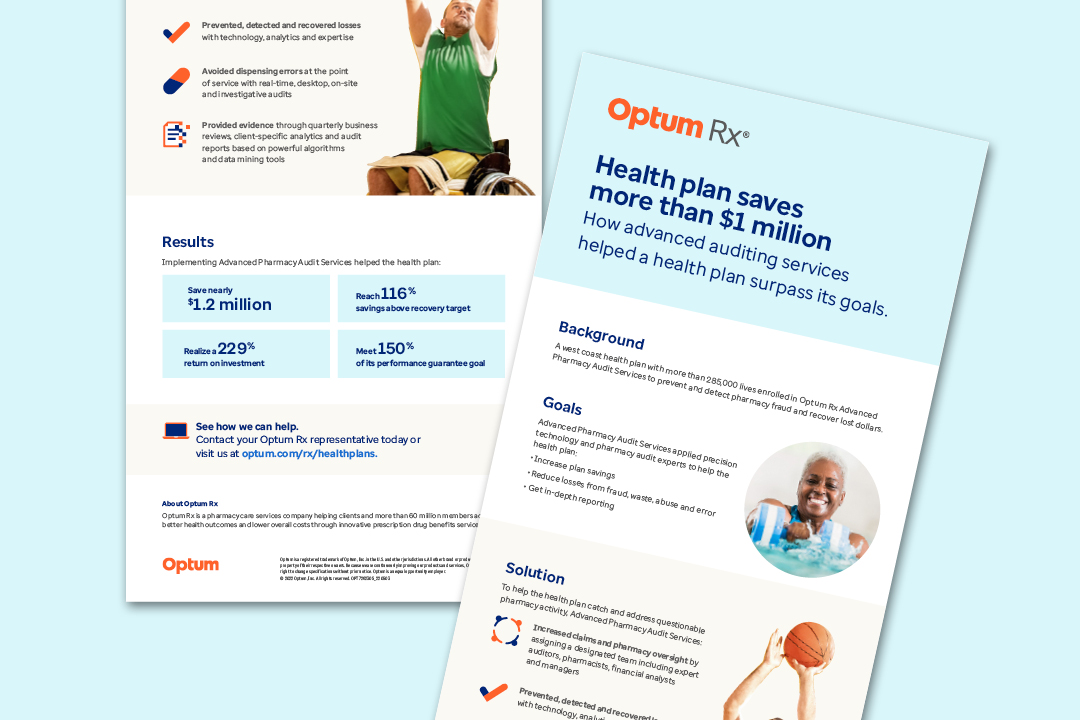
In this case study, a west coast health plan with more than 285,000 lives enrolled in Optum Rx® Advanced Pharmacy Audit Services to prevent and detect pharmacy fraud and recover lost dollars.
Through our audit services, this health plan:
- Increased claims and pharmacy oversight.
- Prevented, detected and recovered financial losses.
- Avoided dispensing errors.
The results included saving more than $1 million.
Related healthcare insights
E-book
This is your employer guide to reducing your healthcare spending.
Case study
Learn how a third-party administrator’s client improved health outcomes and lowered costs.
Article
Hear from a leader's perspective on how to manage polypharmacy.


![Managing Diabetes Gains an 8:1 ROI [Case Study]](/content/dam/optum4/resources/images/wf8630361-1158622494-diabetes-investment-1080x720.jpg)
